Credit: Abscent84 via Getty Images.
Pharmaceutical greed is driving the health care system. It leaves Black folks with diabetes at risk of worsening health outcomes and death.
By Anissa Durham
This is part three of “Life or Debt,” Word In Black’s drug price series, exploring the ways Black folks living with chronic disease are forced to manage an expensive health care system. Read the series.
“If my daughter goes 72 hours without insulin, she will die.”
That’s what Tracy Ramey, a Columbus, Ohio mom says of her 12-year-old daughter who has Type 1 diabetes. As a volunteer diabetes advocate, she wants policymakers and politicians to understand the looming death that often hangs over people living with diabetes. This is partly because pharmaceutical companies can charge what they want for prescription drugs.
Three pharmaceutical companies control 90% of the world’s insulin market — Eli Lilly Co., Novo Nordisk, and Sanofi. The drug giants compete for access to insured patients, but this often leaves patients paying even more.
“Insulin only costs about $4 to make,” Ramey says. “But it costs about $200-$300 per vial of insulin. My daughter goes through four vials a month, and she uses an insulin pump.”
Courtesy of Tracy Ramey.
The United States federal government has historically not been allowed to negotiate directly with pharmaceutical companies on prescription drug prices, says Georges C. Benjamin, executive director of the nonprofit American Public Health Association. Negotiations typically happen between a pharmaceutical company and insurance companies.
“Nobody pays the full rack rate for anything in medicine,” Benjamin says. “Another problem we have is that a lot of those negotiations aren’t very transparent.”
But negotiation practices just recently changed — a bit.
The Inflation Reduction Act gave insurance companies the power to negotiate prescription drug prices directly with drug companies. As a result, out-of-pocket costs for insulin were capped at $35 per monthly prescription for Medicare Part D enrollees. This applies to patients who are 65 or older or younger people with end-stage renal disease or amyotrophic lateral sclerosis.
According to data from 2013, the most recent data available, 2.3% of Medicare beneficiaries 65 years and older reported managing Type 1 diabetes. The problem is the $35 co-pay cap has had little to no effect on most Americans — including Ramey.
The Failures of Health Care
With more than 45 years of experience as a physician, Georges knows how groundbreaking and vital prescription drugs are for patients. But preventative care, he says, can keep patients from having to use drugs in the first place. That’s even more important with diabetes, which can affect every organ in the body
The U.S. doesn’t invest enough resources to prevent chronic illnesses, Georges says. It also doesn’t help that it’s the only industrialized nation that doesn’t have universal health care. This forces Americans to navigate privatized health insurance, a fluctuating drug price system, and access to care on their own.
Related: Have Diabetes? This Guide Breaks Down Insurance and Big Pharma
“The health system is a market failure,” Georges says. “Some parts are heavily regulated, some parts are lightly regulated, and prices are often at the benefit of whoever the seller is.”
In a KFF Health Tracking Poll, 67% of U.S. adults in fair or poor health were more likely to say they experienced a problem using their health insurance. Issues include patients being denied claims for reimbursement, problems finding an in-network provider, and pre-authorization problems.
With or without insurance, there is no free market in the drug industry. This means pharmaceutical companies often price drugs well above what a competitive market would allow, according to the American Institute of Economic Research.
“Why insulin is so much more expensive in the U.S. than in other countries is simply because of pharmaceutical greed,” says Shaina Kasper, policy advocacy director of T1International, a non-profit organization advocating for people living with Type 1 diabetes.
Americans are left at the mercy of the existing health care system and the drug market.
Kasper herself lives with Type 1 diabetes and pays about $7,000 a year for prescriptions and supplies, even though she has a good health insurance plan. She says this system exploits people like herself who are reliant on insulin to live.
“There’s this cartel-like behavior between these three companies,” she says. “They pack their pockets at the expense of patients’ lives.”
The Toll of Diabetes
Ramey’s daughter has lived with Type 1 diabetes since she was six. In November, she quit her teaching job because her daughter was admitted to a behavioral health facility.
Undated photo of Tracy Ramey and her daughter. Courtesy of Ramey.
“She is in a space right now where she isn’t confident in herself. And she hates diabetes,” Ramey says. “Diabetes has a huge mental health impact on her life.”
The pre-teen deals with stigma and often doesn’t tell people at school she deals with the autoimmune disease, her mother says. Her daughter is afraid they will blame it on her weight — which is a contributing factor to a Type 2 diabetes diagnosis.
During the early months of Ramey’s unemployment, she was told to wait to apply for Medicaid — out of fear she would get denied coverage if they found out she had savings in the bank. Between the ambulance rides, hospitalization due to potential sepsis, and a behavioral health facility stay, Ramey’s initial bill was $15,000.
After wiping out her savings in January, she applied for Medicaid. But coverage didn’t kick in until early March. Now, she received a final notice of $36,029 from the children’s hospital.
Unfortunately, Ramey isn’t alone. About a quarter of U.S. adults currently have medical or dental debt that is past due or they are unable to pay.
“It’s very disheartening, but that’s why I fight as hard as I can,” Ramey says. “No one with diabetes asked for it. I didn’t ask for gestational diabetes. I didn’t ask for Type 2 diabetes. And diet and exercise are not a valid justification for people to die.”
The mental health toll isn’t the only toll Black folks deal with when living with diabetes.
To avoid running out of insulin, Georges says he’s seen patients skip, split, and share a dose. But this can leave patients in even worse conditions due to the complications. African Americans coping with diabetes, Benjamin says, have an “enormous and terrible” history of going blind, going on kidney dialysis, and limb amputations as a result of untreated diabetes.
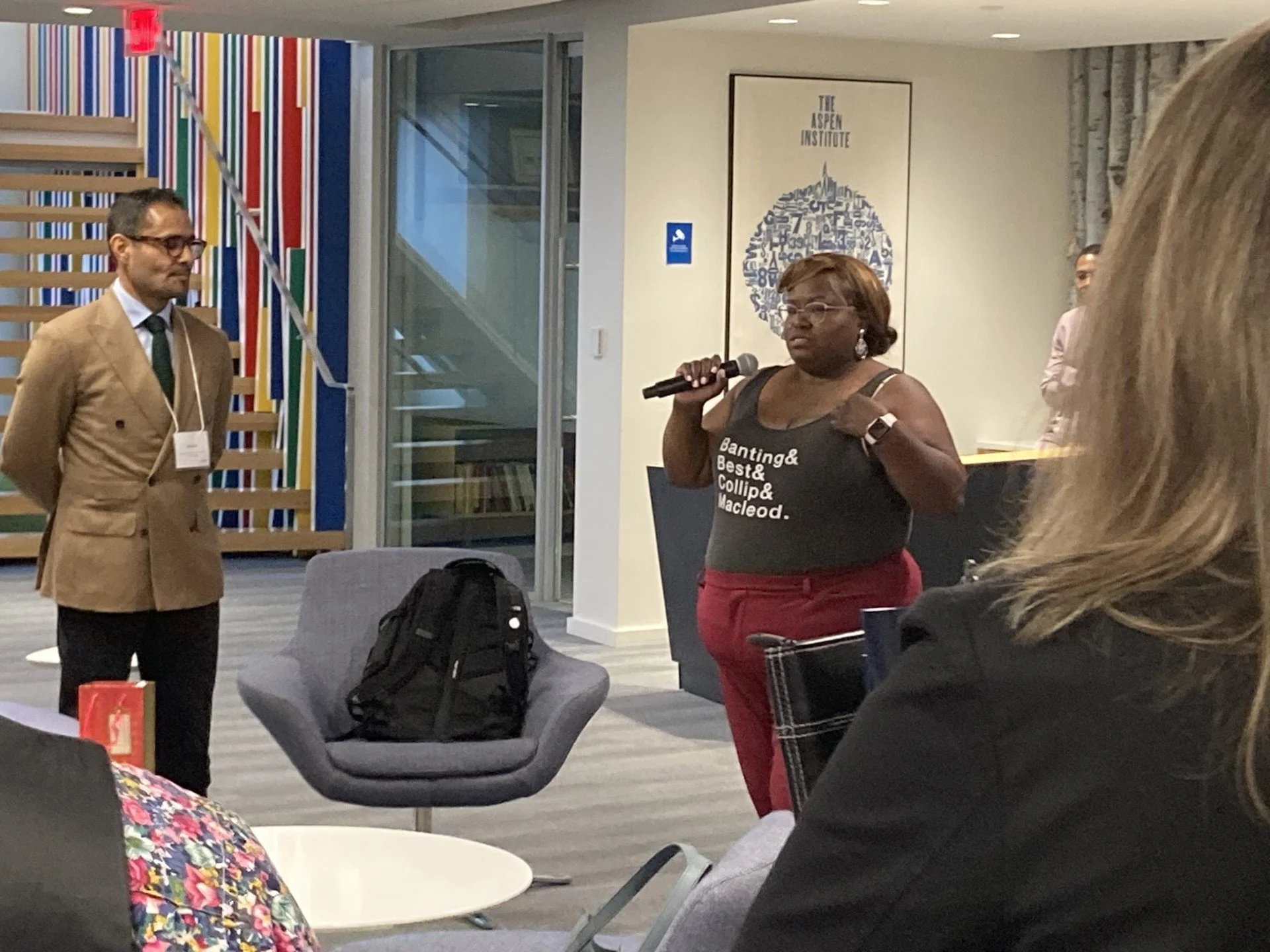
Courtesy of the Georges C. Benjamin.
In medical terms, patients are considered non-compliant when they don’t take their medication as advised; he explains — “quite frankly, the reason they could not comply is because they couldn’t afford the medication.”
For those who are uninsured, people are left to pay full price for everything they access in the health care system. Georges considers it a “nightmare.” Although some pharmacies offer discount programs, he says patients are met with a stack of paperwork that usually needs to be renewed regularly.
“Nothing we do is driven towards patients. We talk a good game about being patient-centered — at the end of the day, everything is driven by money,” he says. “The way the system is designed does not serve individuals.”
Solutions to a Toxic Ecosystem
Jonathan Watanabe, director of the Center for Data-Driven Drugs, Research, and Policy at the University of California, Irvine, and Clinical Pharmacist, says it’s an American phenomenon for patients to experience medical bankruptcy.
The negotiation practices that take place between pharmaceutical companies and other for-profit firms have historically been protected as confidential. This means the dealmaking that happens is hidden and, in essence, legally protected from public knowledge. The lack of transparency allows pharmacy benefit managers, drug makers, wholesalers, insurance companies, and other players to operate without oversight on cost in many situations.
“There is not one single bad actor,” Watanabe says. “This is an ecosystem. We’ve got to start modifying the ecosystem to improve outcomes.”
Credit: Halfpoint Images via Getty Images.
What’s the solution?
Everyone interviewed in this story pointed to policy.
Watanabe suggests emphasizing to policymakers that improved access to insulin and other drugs has societal benefits. For example, if there were more focus on preventative care for underserved populations, it would save patients and the health care system expensive episodic costs of care.
The message is clear: access would benefit society on a grander scale, he says. Individuals with health insurance coverage are more likely to receive an earlier diagnosis and treatment, which contributes to improved health outcomes, according to the American Hospital Association.
What it boils down to is equity.
“How you were born should not decide the care you receive,” Watanabe says. “If you’ve got care that people can’t access, it has no benefit.”